In Health Care, Small Changes Can Have Massive Impacts
By Scottie Barsotti
Heinz College economist Martin Gaynor has some ideas about how to fix the markets that underpin American health care. As part of recent Congressional testimony he rolled out new policy recommendations to attack systemic problems in health care with targeted solutions to reduce costs while maintaining or improving quality.
The United States spends a lot of money on health care each year. Like, a lot a lot. More than any other wealthy nation per capita, and it’s not even close. Nearly one out of every five dollars spent in the U.S. is spent on health care. You might think that all that expense would mean we have the best quality health care in the world—in reality, health outcomes in the U.S. lag behind other countries.
The U.S. health sector is a huge, sprawling, complicated network of providers, payors, and policies that can seem both hopelessly complex and stubbornly resistant to change. And while that’s true in some respects, it’s not to say that improving the system would be impossible. In fact, the U.S. health care sector is so mammoth, that even seemingly incremental fixes can have major impacts.
Heinz College economist Martin Gaynor has identified some of those fixes.
“There are some very simple, straightforward things we can do that can really make a difference,” said Gaynor.
On July 15, Professor Gaynor will be part of an expert panel on health care at Heinz College, moderated by Margot Sanger-Katz of The New York Times. Other panelists include Katherine Baicker from the University of Chicago, Zack Cooper from Yale University, and Shelley White-Means from the University of Tennessee. The panelists will discuss several major issues facing the American health system and propose solutions.
Gaynor has extensively studied competition and consolidation in the U.S. health care market, a growing problem nationwide. He has testified before Congress that in markets where there is greater consolidation and less competition (many places in the U.S. only have one or two large health systems that dominate the local market), prices tend to increase substantially, without any improvements in quality (and in some cases reductions in quality).
Gaynor remarks that health care consolidation has accelerated in recent years, negatively affecting consumers. Consolidation between close competitors causes prices—and health care spending—to go up. When that happens, the premiums that insurers charge to employers also go up, and workers end up footing the bill, either through reduced wages, paying a higher share of premiums, reductions in insurance coverage, or in some cases all three.
One solution he proposes is a relatively minor change to the way Medicare pays for physician services—something known as “site-specific billing.” Medicare pays physicians a certain rate for seeing patients in their practice. However, if that practice is owned by a hospital, the same fee gets paid to the physician, but Medicare also pays a “facility fee” to the hospital, which can double the cost for the same service.
“That can be very profitable. Site-specific billing is a major factor leading hospitals to acquire physician practices in recent years,” said Gaynor. “It’s a big contributor to market consolidation in health care, which drives up costs. Fixing it would just be a matter of removing this artifact in how Medicare pays.”
Gaynor also refers to a policy called the “340b program,” which subsidizes hospitals for physicians’ drug purchases, as a contributor to this problem.
“Even the most careful planning can have unintended consequences. Now that we know these problems exist, and how to fix them, they can be fixed,” said Gaynor.
Along with his colleague Zack Cooper from Yale University, Gaynor put forth several policy recommendations, which he’s recently shared with regulators and members of Congress. These policies, which Cooper and Gaynor estimate could amount to 2 percent of private health spending when taken together, include:
- Increasing funding for antitrust enforcement agencies: Gaynor notes that federal antitrust agencies, such as the Antitrust Division of the Department of Justice and the Federal Trade Commission, are under-resourced, and their level of funding has not kept pace with mergers.
- Amending the Federal Trade Commission Act to allow the FTC to take enforcement action against anticompetitive conduct by not-for-profits:Gaynor points out that the majority of hospitals in the United States are nonprofit firms, which prevents the FTC from taking action against anticompetitive practices that harm consumers.
- Introducing site-neutral billing in Medicare:As mentioned above, Medicare’s “site-specific” payment policies have inadvertently led hospitals to acquire physician practices, leading to an increase in vertical integration and less competition in local markets.
- Amending the 340b program so dollars follow the patients: Gaynor suggests that by having such a subsidy follow individual patients, rather than the purchaser or prescriber of the drug, it would further blunt the incentive for hospitals to acquire independent physician practices.
- Having states examine laws and regulations that unintentionally reduce or thwart competition: States have a number of laws, including licensing, certificate of need, scope of practice, and certificates of public advantage, that, while well intended, act to thwart new competitors and harm competition. These laws and regulations should be reexamined and narrowly tailored to achieve their goals of protecting the public while not harming competition.
- Strengthening existing antitrust enforcement laws:Gaynor believes lawmakers should enact legislation that strengthens existing antitrust laws. He says that current standards place too high a burden on plaintiffs, like DOJ and FTC, which can cause these agencies not to bring some antitrust cases at all.
- Reporting requirements for small mergers and acquisitions:Gaynor suggests that all mergers should have reporting requirements, but presently deals under $50 million do not have reporting requirements. This causes many of the aforementioned acquisitions of physician practices to go unreported, which is problematic for antitrust monitoring and enforcement.
- Having the FTC and DOJ issue revised guidelines for antitrust enforcement in health care: These guidelines were issued in 1996. Gaynor says much has changed since that time, and a refreshed and revived set of health care guidelines will provide important guidance to market participants and courts.
- Establishing a national health care database that has comprehensive, publicly available data on US health care spending, utilization, prices, and ownership: Gaynor calls this a critical investment in our national infrastructure that will make vitally important information available to businesses, government, and citizens.
Professor Gaynor is quick to note that such solutions would not fix everything—health care is much more complicated than any one single issue. But that’s precisely why changes that seem small can make such a difference collectively.
“We spend 3 trillion dollars on health care each year. Even if something saves you a fraction of a percent? I’ll take it,” said Gaynor.
“In the long term, the question of what health system would be best is a question we should engage with. In the meantime, we have a market-based system in the U.S., so making these markets work as well as they can is to the benefit of American citizens.”
Small Steps, Big Impacts
Gaynor is part of a nationwide effort to pinpoint those kinds of health care solutions that save a a percent here, a percent there. It’s called the “1% Steps for Health Care Reform Project.” The group, made up of leading academics in the health care space, prescribes small tweaks to the U.S. health care system that could save billions, even tens of billions of dollars in spending without affecting quality.
Savings like that could add up quickly. But it’s not just about the money.
Where there’s less competition, patients (particularly patients with mobility issues) have fewer choices. And Gaynor adds that markets with less competition not only see higher prices, they also tend to deliver lower quality, which can show up as increased mortality rates among certain patient groups.
“When you’re dealing with very sick patients, they’re very vulnerable. In health care quality, little things matter, and lots of little things can add up,” said Gaynor. “If a hospital isn’t pushed by tougher competition and consumers don’t have a real choice, it’s feasible that things would start to slip in ways that cumulatively affect quality.”
As is the case with any system, changes in one area could have cascading effects. Gaynor believes consolidation has a corrosive quality that eats at many other parts of the system, and that improving competition could have ripple impacts.
“Consolidation is not the whole of the problem, but it is a big part of the puzzle that drives other issues.”
Gaynor expects consolidation and competition to be important points of conversation at the upcoming Heinz College-NYT panel.
Learn more about the event and register to attend below.
Mission Impossible? How to Fix U.S. Healthcare
Can U.S. healthcare be saved, or is the patient beyond all hope?
Moderated by Margot Sanger-Katz of The New York Times
Thursday, July 15 (Register by Wednesday, July 14)
1:30-2:30 p.m. ET
Zoom Webinar
Registration is required for this free event. Register by Wednesday, July 14. Zoom login information will be provided via a confirmation email.
 Margot Sanger-Katz, Moderator
Margot Sanger-Katz, Moderator
Healthcare Correspondent, The Upshot
The New York Times
 Katherine Baicker
Katherine Baicker
Dean and Emmett Dedmon Professor
Harris School of Public Policy
University of Chicago
 Zack Cooper
Zack Cooper
Associate Professor, Institution for Social and Policy Studies
Yale School of Public Health
Yale University
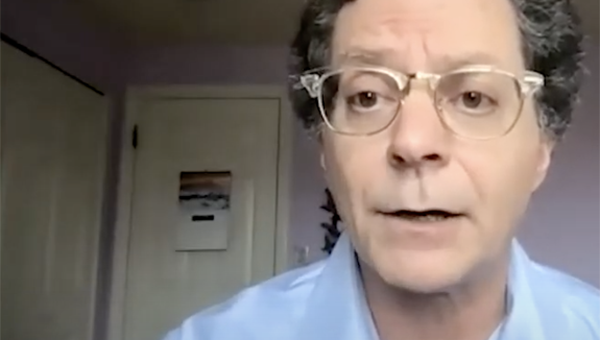
 Martin Gaynor
Martin Gaynor
E.J. Barone University Professor of Economics and Public Policy
Heinz College of Information Systems and Public Policy
Carnegie Mellon University
 Shelley White-Means
Shelley White-Means
Professor and Executive Director of Consortium for Health Education
Economic Empowerment and Research (CHEER)
University of Tennessee Health Science Center